Opioids are a class of drugs that are commonly prescribed for pain relief. They are the product of the opium poppy plant, typically grown in South America and Asia.
A growing body of research shows that opioid drugs may lead to blood clots in the body that may result in potentially life-threatening issues such as heart attack and stroke.
Here you will learn more about:
- how blood clots form and why they’re dangerous
- the effects of opioid painkillers and illicit heroin on the cardiovascular system
- signs and symptoms of a blood clot
- treatment programs for opioid use disorder (OUD)
What Is A Blood Clot?
Blood clots are a normal and essential function of the body. When they form abnormally, however, they can lead to potentially harmful or deadly conditions.
How Blood Clots Form
Blood clots form when a collection of cells, platelets, and proteins in the blood stick together to form a mass. Blood clots commonly form in the body to help stop bleeding when you get hurt.
When the injury stops bleeding, most blood clots are broken down. Sometimes, however, the clot will not get fully broken down or will form in an abnormal area where there’s no injury, leading to serious health problems.
Why Blood Clots Are Dangerous
When blood clots don’t break down as they should, they will move through the blood until they get stuck in a narrow passage in an artery. When a clot gets stuck like this, it’s called an embolus.
An embolus becomes extremely dangerous when it gets stuck in a cerebral or coronary artery, or when they become lodged in other organs like the kidneys and lungs because it will cut off the oxygen supply to vital organs.
How Opioid Use Affects The Cardiovascular System
Legal opiate medications such as oxycodone (OxyContin), hydrocodone (Vicodin), morphine, and the synthetic opioid fentanyl are powerful tools to stop chronic pain or acute pain after surgery.
When opioid drugs are responsibly prescribed, the clinician will closely monitor the effects they are having on the body, reducing the risk of blood clots or other adverse reactions.
People who use illicit opioids such as heroin are at a much higher risk for damage to the cardiovascular system. Blood vessels may become clogged due to substances in heroin not dissolving properly.
Atrial Fibrillation
The American Heart Association (AHA) has found that people who use opioids even at a low dose are 34 percent more likely to develop Atrial Fibrillation, also known as AFib.
AFib occurs when the heartbeats in the upper and lower chambers of the heart are out of sync, and as a result, the blood doesn’t move evenly to the arteries. Blood clots can form and enter an artery that leads to the brain, causing a stroke.
Vein Scarring And Bacterial Infections
People who chronically inject heroin into their veins are at high risk of causing scarring in the veins used for injection, or bacterial infections in the veins and heart valves.
Damaged veins and heart valves may facilitate the growth of blood clots due to blood flow being affected by damaged tissue.
Deep Venous Thrombosis (DVT)
One of the most common places for blood clots to form is in the arteries deep within the leg, also called Deep Venous Thrombosis (DVT) or venous thromboembolism.
Nearly half of people who develop DVT will have no symptoms. If symptoms do show up, they may include leg pain, skin redness, and swelling in the leg.
Pulmonary Embolism (PE)
A pulmonary embolism occurs if a blood clot reaches the lung and causes a blockage. A blockage in the lung will lower the oxygen level in the blood and damage other organs.
Common symptoms associated with PE include shortness of breath, rapid breathing, chest pain, and coughing up blood.
The Signs And Symptoms Of A Blood Clot
Blood clots may appear in multiple places in the body, and the symptoms for them will be dependent on where the clot mass is.
Common symptoms of a blood clot may include:
- abdominal pain, nausea, and vomiting
- drastic changes in blood pressure
- swelling, tenderness, warmth, or pain in the arm or leg
- slurred speech, vision problems, seizures, and headache
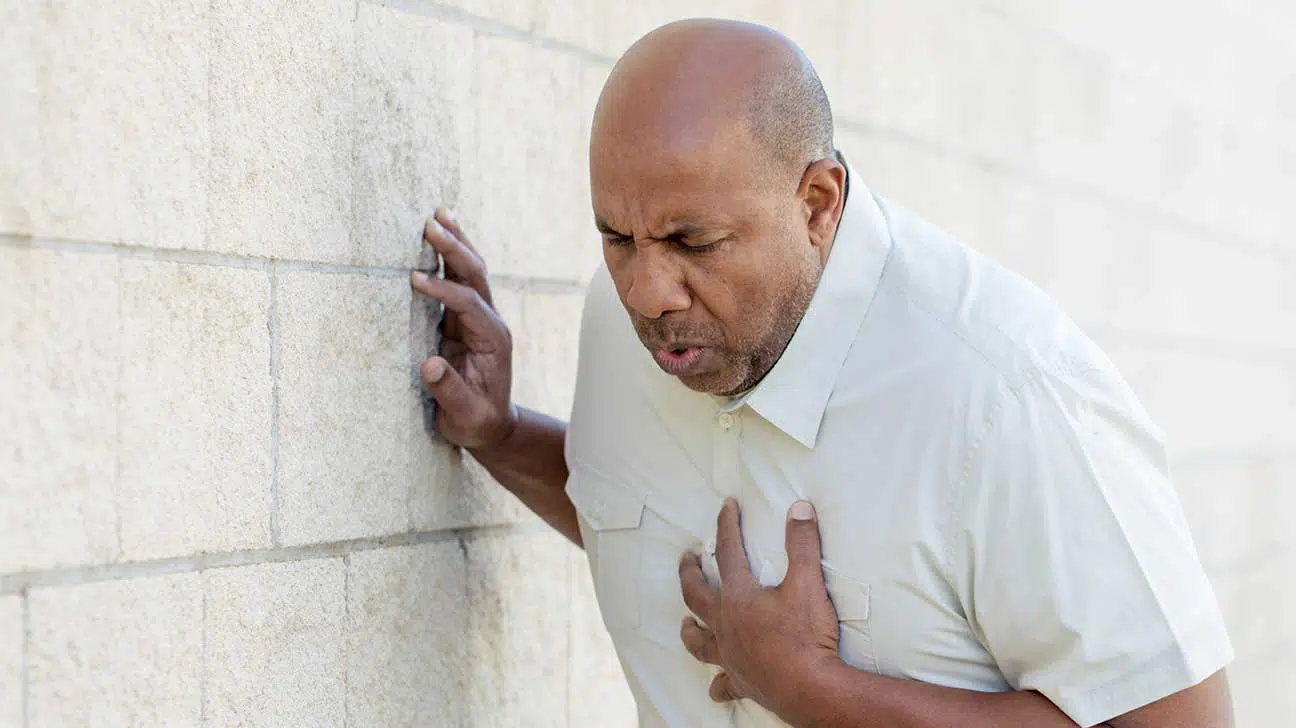
- heavy chest pain, shortness of breath, sweating, and other symptoms of a heart attack
It’s important to seek the guidance of a healthcare provider or call the emergency department immediately if you or a loved one are using opioids and experiencing any of the above symptoms.
When discovered early, blood clots may be treated with blood-thinners, anticoagulants, surgical procedures, or blood clot dissolvents called thrombolytic.
Treatment Options For Opioid Addiction
If you or someone you care about is addicted to prescription opioids or uses heroin intravenously, help is available in the form of evidence-based addiction treatment.
Treatment services may include:
- medication-assisted treatment (MAT)
- dual diagnosis treatment for co-occurring mental health disorders
- medically monitored opioid detox
- inpatient treatment programs
- outpatient care
- individual, group, or family counseling
Opioid drug use can put you at a greater risk for blood clots and a host of other health disorders.
Receiving treatment for opioid use disorder will help lower your increased risk and put you on the path to sobriety.
Find A Rehab Center For Opioid Drug Abuse
Call or visit our helpline today for more information on risk factors for opioid addiction and treatment options available near you. Our team can also provide referrals for medical advice.


