What Is Polysubstance Abuse?
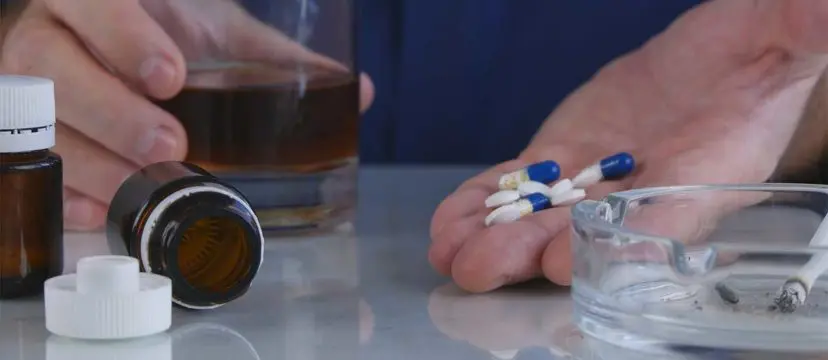
Polysubstance abuse, also called polydrug use, occurs when a person abuses more than one substance (or drug) at a time. The abuse can occur with both drugs in one incident or at separate times during the same period of abuse. A person may, for example, take two drugs together for their intended opposing effects, or may take one drug after another to counteract the effects of the first.
Polysubstance abuse comes with a unique set of risks in addition to the risks and dangers associated with each substance, including increased risk of overdose, increased mental health issues or chance of developing such issues, and risky behavior due to acute intoxication, which can lead to serious injury or accidents.
Treatment for polysubstance abuse and addiction must be comprehensive and based on the individual’s needs.. Individuals in recovery should receive treatment for any and all substance use disorders to ensure the greatest chance at achieving sobriety and entering recovery fully-equipped to avoid relapse and live a full, healthy life.
Polysubstance Abuse Vs. Addiction
It’s important to first understand the difference between polysubstance abuse and addiction. Abuse of a substance can take a few different forms. For instance, if a substance is illicit (illegal), such as heroin or cocaine, then use of it is always considered abuse.
Are you or a loved one suffering from addiction?
Don't wait, get the best treatment options today!
Call Now: (888) 407-2072Other forms of abuse occur when a person takes a prescription drug, such as the opioid, oxycodone (OxyContin), or the benzodiazepine, diazepam (Valium), in a way other than intended by doctors. Abuse of prescription drugs include: changing method of administration (such as crushing a pill and snorting it for faster effects), changing dosage, changing frequency of dosage, or taking someone else’s prescription.
If a person abuses a drug for an extended period of time, or a highly-addicting drug several times, addiction can result. Risk of addiction is especially high when abusing multiple substances, as each instance of abuse puts a person at further risk for developing an addiction.
Addiction is a chronic disease which affects the brain and causes relapse. Drugs interrupt brain communication pathways by binding to receptors and altering the processes in the brain. They also cause physical effects which make the person feel a surge of euphoria and other pleasurable effects, prompting the person to seek the drug or drugs again and again.
When a person becomes addicted to a drug, he or she is affected by compulsive drug-seeking and use. With time, the effects of continued abuse take their toll on a person’s psychological, physical, emotional, and behavioral well-being.
Who Is Affected By Polysubstance Abuse?
The National Institute on Drug Abuse (NIDA) explains that addiction, like many other diseases, will affect each person differently. A person’s vulnerability to addiction depends on a number of risk factors, including: aggressive behavior in childhood, lack of parental supervision, lack of or poor social skills, instance of drug experimentation, how available drugs are to a person in their youth, and poverty level.
Other factors include environmental ones, such as the influence of home on a person during their childhood, i.e. if a child has access to a stable home and support from family, he or she will be less likely to fall into addiction.
People who began using substances at an early age are more likely to develop addiction later in life, the NIDA states. How a person abuses a drug is also a factor—when a person abuses a drug by a method of administration that produces instant effects, such as by smoking or injection, he or she is more likely to quickly develop an addiction to it.
It is not known exactly how many people in the United States are affected by polysubstance abuse and addiction. However, one study of more than 69,000 clients in publicly-funded treatment admissions from 1998 to 2004 found that 51.3 percent of admissions reported mono-drug use (abuse of a single drug) while 48.7 percent reported polydrug abuse.
While this may point to a roughly equal number of people abusing multiple substances compared to those abusing one substance, not enough research exists on polysubstance abuse, its effects, or related matters for a full conclusion. In any case, at the least, tens of thousands of people are affected by polysubstance abuse and addiction each year, with a suspected larger number, who become exposed to the risks and dangers associated with these illnesses.
Signs And Symptoms Of Polysubstance Abuse And Addiction
Because each drug affects each person differently, and each person reacts to drugs in his or her own way based on a number of biological and psychological factors, polysubstance abuse can be hard to spot. For example, the signs of abuse of a stimulant, such as cocaine, will differ greatly from signs of abuse of a depressant, such as alcohol. Combining two substances such as this can mask the effects of each, making identifying the specific drug of abuse more challenging.
Signs of abuse can be physical, behavioral, psychological, or external (how drug abuse affects a person’s life). No matter the substance combination, people abusing drugs tend to experience vast changes in one area or more of their health or personal life once drug-seeking and using becomes the top priority due to addiction.
General signs and symptoms of polydrug abuse and addiction include:
- acute intoxication
- extreme hangovers
- increased risky behavior, such as driving while intoxicated
- increased instances of accidents and injuries, such as falls
- violent behavior, such as getting into physical fights
- development of mental health issues, or worsened mental health issues
- signs of physical dependence: experiencing withdrawal symptoms when not using a substance
- signs of tolerance: taking a substance, or multiple substances, more often, increasing the dosage, or needing more to feel the desired “high” or to function
- physical effects, such as signs of intravenous use
- instances of paraphernalia, or items used for drug abuse, such as spoons, lighters, loose powder, pipes, etc.
More specific signs of polysubstance abuse can be found according to the effects of certain polydrug combinations, such as cocaine and alcohol or cocaine and heroin.
Dangers Of Polysubstance Abuse
The dangers associated with polysubstance abuse and addiction occur according to which drugs were abused. Each drug produces certain mind-altering and physical effects, and mixing these effects when combining different drugs can have taxing effects on the brain and body.
Research from Edith Cowan University explains, “Sometimes using some drugs together can lead to greater effects than would be expected from simply adding up the effects of each drug. This is called synergism. It happens when one drug actually makes the other drug work more strongly.”
Abuse of one drug can cause typical effects of abuse for that drug, but when a person abuses another drug at the same time, the effects may be amplified causing increased intoxication. The University goes on to explain that, “as a result, the effects of combined drug use can be very unpredictable and dangerous.”
Polydrug Abuse: Commonly Abused Substances Combinations
The following are common polysubstance abuse combinations and the effects associated with them.
Alcohol And Other Drugs (Benzodiazepines, Opioids, Marijuana, Cocaine, Prescription Drugs)
By itself, alcohol can be a powerful depressant, especially when people binge drink, or consume several drinks in a row on one occasion, or drink heavily. Mixing alcohol with other substances of abuse can be dangerous as combining the two substances can either amplify the effects of both or mask the effects of each.
Alcohol And Cannabis
Mixing alcohol and cannabis (marijuana) can lead to a higher rate of intoxication than if a person were to use either drug on its own. Abuse of both drugs can also lead to increased risky behavior, such as accidents, injuries, getting into physical fights, violence, and increased instance of paranoia.
Alcohol And Stimulants
Mixing alcohol and stimulants, such as amphetamines, methamphetamine, or cocaine, can have dangerous effects. Alcohol is a depressant, meaning it has the opposite effect of stimulants in that it slows body functions. Stimulants work to increase functions, including energy, alertness, and certain body functions, such as breathing and heart rates. Mixing alcohol and stimulants can lead to increased intoxication and increased risk of overdose.
Combining two drugs with opposing effects works to mask the effects of the drugs, causing a person to continue to abuse the drugs, either because they don’t feel the effects as acutely or because they feel as if the effects wear off more quickly. This is especially true for the combination of the stimulant cocaine and alcohol.
Alcohol And Cocaine
Alcohol causes side effects such as: slowed reaction time and reflexes, depression, slurred speech, loss of coordination, reduced breathing and heart rates, and impaired judgment. Cocaine is a depressant that causes opposing effects, including: intense and immediate sense of euphoria, anxiety, paranoia, high energy, alertness, increased body temperature, and increase in taking risks.
While the drugs do not each work to cancel out the other, the person abusing them may feel as if that is what’s happening.
Combining alcohol and cocaine can cause the two substances to mask the effects of each. As a result, the person may continue drinking or taking subsequent doses of cocaine, leading to both increase in acute intoxication and risk of overdose.
Alcohol And Opioids
The National Council on Alcoholism and Drug Dependence states, “a new study warns drinking alcohol while taking powerful opioid painkillers can trigger a potentially deadly respiratory problem.” The study measured the effects of mixing opioid painkillers and alcohol and found that even taking one oxycodone (OxyContin) tablet while drinking moderately increased the risk of respiratory depression (stopping breathing).
Opioids cause an altered perception of pain and a sense of euphoria when abused. The drugs work in the body by reducing certain functions, like breathing and heart rates. While opioids are not depressants, they work to reduce some of the same functions of depressants like alcohol, and combining the two amplifies these effects, which is what can cause stopped breathing.
Stimulants And Other Drugs
Stimulants cause increased heart rate and breathing, energy surges, intense euphoria, alertness, and, sometimes, increased sense of confidence. Combining stimulants and other drugs can drastically enhance the effects of the drugs, causing increased risk for certain medical conditions, such as heart attack, stroke, and fatal overdose.
Cocaine And Heroin (Speedball)
Cocaine can cause rapid and intense “highs,” however, these effects are often followed by an even more intense “low” period of depression, anxiety, and other negative effects. The National Institute on Drug Abuse for Teens explains that when combining cocaine and heroin there is a “push-pull” reaction; cocaine is a stimulant, while heroin, an opioid, works as a depressant with its opposing effects.
The goal of abuse is a more intense high with a less intense low. The NIDA for Teens explains that, unfortunately, this type of abuse can intensify the effects of each drug while greatly increasing risk of respiratory depression and overdose. Learn more about “The Dangers Of Mixing Heroin With Cocaine (Speedballing)”.
Cocaine And Ecstasy
Cocaine and ecstasy are both stimulants which some people may abuse together to try to enhance the expected high. Yet both drugs increase a person’s heart rate and other functions, greatly increasing a person’s risk of heart attack and stroke. The same risk goes for mixing other stimulants as well, including amphetamines, such as Adderall, and methamphetamine (meth).
Opioids And Benzodiazepines
Benzodiazepines are medications used to treat seizures, insomnia, and anxiety, and they include alprazolam (Xanax) and diazepam (Valium). In 2016, the U.S. Food and Drug Administration issued a warning that mixing opioids, like heroin or hydrocodone (Norco, Vicodin), with benzodiazepines could cause a dangerous drug interaction.
CBS News reported that the FDA conducted a review which found that many patients who were prescribed opioids were also prescribed benzodiazepines, despite the dangers. Benzodiazepines work like a sedative in the body, while opioids cause central nervous system depression. Combining opioids and benzodiazepines can cause fatal consequences, including coma and death.
Prescription Drugs And Other Substances
Many people may not be aware of the risks associated with mixing prescription drugs with other substances, but, depending on the medication, the dangers and risks can be very real and sometimes fatal. This can also be true for non-prescription, or over-the-counter, medications in some instances.
Prescription Drugs and Alcohol
Alcohol can render a prescription medication useless or can even make the medication harmful or toxic to the body. At the very least, mixing alcohol and prescription drugs may cause the following effects: headaches, nausea, vomiting, drowsiness, fainting, and loss of coordination. In the worst instances, mixing medications with alcohol can put a person at risk for internal bleeding, heart issues, and difficulty breathing.
Abuse Of Multiple Prescription Drugs
People who are prescribed multiple medications may end up abusing them at the same time. Mixing certain combinations, such as anti-anxiety medications, benzodiazepines, and painkiller opioids can have dangerous effects. Abusing certain prescription drugs comes with risk of fatal overdose, but abusing more than one prescription drug at a time greatly increases this risk.
Polysubstance Abuse And Co-Occurring Disorders
In addition to the physical risks of polysubstance abuse and addiction, such as overdose, abusing more than one substance at a time may worsen the symptoms of a mental disorder or contribute to the development of one.
Co-occurring disorders, formerly called a dual diagnosis, occur when a person suffers with both a substance use disorder and a mental health disorder. According to the National Alliance on Mental Illness (NAMI), either the substance use disorder or the mental health disorder can occur first, and having one disorder may make a person more likely to develop the other.
For example, people experiencing mental health issues, such as anxiety or depression, may try to self-medicate by abusing drugs or alcohol. However, research has found that instead of helping alleviate the symptoms of the mental health disorder, substance abuse tends to make them worse.
As of 2014, 7.9 million people had a co-occurring mental disorder and substance use disorder, NAMI reports. Treating co-occurring disorders can be more challenging, as it’s important that both disorders are properly diagnosed and treated or a person’s recovery outcome may be affected.
A comprehensive treatment plan within an inpatient drug rehab center can help individuals overcome polysubstance abuse and learn to manage their mental disorder.
Medical Detox For Polysubstance Abuse And Addiction
Depending on the substance of abuse, a person may require a medical detoxification before proceeding to addiction treatment. Alcohol, barbiturates, benzodiazepines, and opioids can all cause physical dependence, which means when a person tries to go off the drugs, they experience uncomfortable and, in some cases, dangerous withdrawal symptoms.
Depending on the severity of abuse and duration of addiction, a person may need a medical detox, which involves constant monitoring and medical support.
Within a medically-supervised detox program, a person will be monitored for vital functions, have access to medication as needed, and receive medical aid depending on their individual needs, such as nutritional and vitamin deficiency support.
Some drugs can cause life-threatening forms of withdrawal, including alcohol, while others aren’t always life-threatening but can be so uncomfortable a person is likely to relapse without medical help in detox.
Detoxification allows a person to flush out harmful toxins from polysubstance abuse and prepare for formal treatment and recovery.
Treating Polysubstance Abuse And Addiction
While a medical detox may be the necessary first phase of addiction treatment, a formal treatment program should always follow detox to ensure the best chance for a successful recovery outcome, especially in the case of polysubstance abuse and addiction.
Inpatient addiction treatment programs can provide the environment an addicted individual needs to make a great change in their life. Learning to manage addiction can be difficult, and with abuse of more than one drug, a person will likely need an intensive program tailored to their specific needs.
Many drug rehab centers now provide dual diagnosis treatment programs to target the unique needs of people in recovery from more than one disorder. A full assessment of both disorders and a treatment plan that takes into account the individual’s medical history, as well as other factors, is necessary for treatment success.
Finding the right addiction treatment program in a facility that cares about and supports each individual can be detrimental to a person’s recovery outcome. Continued care for polysubstance abuse and addiction is as important as the treatment itself, so when finding a drug rehab center, it’s important to consider this factor as well.
Learn more about polysubstance abuse and addiction treatment and the best rehab centers which provide it.
Sources:
- CBS News — Mixing opioids and popular sedatives may be deadly
- Edith Cowan University — Polydrug use
- National Alliance on Mental Illness — Dual Diagnosis
- National Council on Alcoholism and Drug Dependence — Mixing of Opioids and Alcohol Make for a Dangerous Cocktail
- National Institute on Alcohol Abuse and Alcoholism — Mixing Alcohol With Medicines
- National Institute on Drug Abuse — Drug Abuse and Addiction, Misuse of Prescription Drugs
- National Institute on Drug Abuse for Teens — Real Teens Ask About Speedballs


